This factsheet is for people who have fatty liver disease or who would like more information about it.
The term fatty liver disease covers a range of conditions beginning with fat building up in the liver. It can be caused by drinking too much alcohol, or it can be unrelated to alcohol.
About fatty liver disease Symptoms of fatty liver disease Causes of fatty liver disease Diagnosis of fatty liver disease Treatment of fatty liver disease Preventing alcoholic liver disease Preventing non-alcoholic fatty liver disease Questions and answers Related topics Further information Sources About fatty liver disease
A healthy liver contains little or no fat. However, sometimes fat molecules called triglycerides begin to accumulate in the liver cells. This is called fatty liver.
One of the reasons you can develop fatty liver disease is by drinking too much alcohol. This is termed alcoholic liver disease (ALD).
Fatty liver can also be caused by other conditions, including being overweight or obese. When you develop a fatty liver unrelated to alcohol it is called non-alcoholic fatty liver disease (NAFLD).
Developing a fatty liver is becoming more common because of rising obesity levels. At least four out of five obese people are thought to have fatty liver.
In the USA, an estimated 25 to 35 percent of the population have a fatty liver. In the rest of the world, the incidence is thought to be slightly lower. In the UK, around one in five are estimated to have a fatty liver.
Symptoms of fatty liver disease
 Fatty liver disease exists across a spectrum. Simple fatty liver is called steatosis. It often doesn’t have any symptoms. However, about half of all people with steatosis may notice some symptoms including:
Fatty liver disease exists across a spectrum. Simple fatty liver is called steatosis. It often doesn’t have any symptoms. However, about half of all people with steatosis may notice some symptoms including:
feeling tired all the time generally feeling unwell discomfort in your upper abdomen near your liver (at the base of your right rib cage) Although in most cases steatosis is harmless, having fat in your liver can sometimes cause it to become inflamed. This only happens in a small number of people who don’t drink alcohol.
An inflamed liver in someone who doesn’t drink is called non-alcoholic steatohepatitis (NASH). In someone who drinks, this is called alcoholic hepatitis.
Both NASH and alcoholic hepatitis are more likely than steatosis to make your liver swell, causing discomfort or pain. Other symptoms that may indicate fatty liver or liver disease include:
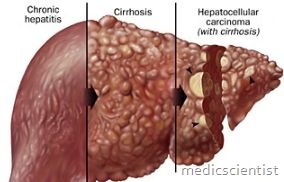
itchy skin vomiting blood dark black faeces bruising easily confusion or poor memory physical signs like yellow skin, wasted muscles, mottled palms Having a badly inflamed liver (NASH or alcoholic hepatitis) for a long time can cause scar tissue to form in the liver. This is called fibrosis.
Continued fibrosis can lead to cirrhosis of the liver. This is when nodules of smooth liver tissue become hardened and scarring continues. Damage done by cirrhosis is irreversible.
NASH is one of the biggest causes of liver cirrhosis. About one in every five people with NASH develop cirrhosis within ten years.
Cirrhosis leads to more severe symptoms of liver disease, including ascites, the build up of fluid in your abdomen, and oedema, a build up of fluid in your bodies tissue – most commonly causing swelling in the hands, legs or feet.
A liver with cirrhosis will not become healthy again. If the underlying condition causing cirrhosis is treated, the damage can be greatly limited. However, if it is allowed to progress and all the cells in the liver become unhealthy, the liver will fail completely. This is fatal. If your liver is about to fail, you will need a liver transplant.
Causes of fatty liver disease
Fatty liver can occur at any age. Fatty liver disease can be caused by drinking too much alcohol. This is called alcoholic liver disease. This describes a spectrum of liver damage from steatosis, to an inflamed liver, to fibrosis and finally cirrhosis.
When fatty liver isn’t linked with alcohol, it can be caused by a number of conditions. However, the progression of the disease is the same. These conditions include the following.
Being overweight or obese
Most people who have fatty liver disease are overweight or obese. Overweight means having a BMI of 25.0 to 29.9. Obese means having a BMI of 30.0 or more. Type 2 diabetes. Insulin resistance, which is linked with the onset of type 2 diabetes. Hyperlipidaemia. This is when you have high levels of cholesterol or triglyceride fats in your bloodstream. High blood pressure. Long-term treatment with certain medicines is associated with fatty liver. For example, tamoxifen (used to treat breast cancer), prednisolone and hydrocortisone (used to treat inflammation), amiodarone (used to treat irregular heart beats), premarin and ortho-est (synthetic hormones used for HRT) and methotrexate (used to treat arthritis). Protein malnutrition. For example, if you were on a drip and unable to eat food. Metabolic syndrome. This is when you have a group of related disorders that are all risk factors for fatty liver, including type 2 diabetes, obesity (especially around the centre of your body) and an abnormal lipid (cholesterol and triglyceride) profile. Some other metabolic problems. Acute Fatty Liver Disease is a very rare complication that can occur during pregnancy or when caused by certain toxins. It can quickly lead to liver failure so needs rapid treatment.
Diagnosis of fatty liver disease
You doctor can diagnose fatty liver disease based on asking you about your symptoms and carrying out certain tests. Some example tests you might have include:
Blood tests
You might have tests to check your liver function and monitor your iron, glucose, cholesterol and triglycerides levels. Although no one lab test can confirm fatty liver disease, some tests can indicate if it is likely.
Imaging
Some scanning methods may identify fatty liver.
Ultrasound. An ultrasound scan uses sound waves to produce an image of the inside of the body/or part of the body. Computed tomography (CT). A CT scan uses X-rays to make a three-dimensional image of the body/or part of the body. Magnetic resonance imaging (MRI). MRI uses magnets and radiowaves to produce images of the inside of the body. Although imaging methods such as ultrasound, CT and MRI can indicate fatty liver disease, they can’t distinguish between simple fatty liver (steatosis) and an inflamed liver such as NASH.
Biopsy
A liver biopsy is the only way to conclusively confirm a diagnosis of NASH. A biopsy is a small sample of tissue. It is taken using a very fine hollow needle that is fed through your skin and into your liver to take a small sample of cells. The sample is then sent to the laboratory for analysis.
Treatment of fatty liver disease
If you have alcoholic liver disease, you need to completely stop drinking any alcohol. If you don’t the condition is likely to progress to the more serious stages of alcoholic liver disease. While cirrhosis is irreversible and likely to need a liver transplant, stopping alcohol consumption may completely reverse simple fatty liver (steatosis).
Doctors are yet to agree on a specific treatment for fatty liver disease. However, if you have fatty liver disease, but don’t drink alcohol, there are a number of things doctors think may improve your condition.
Treating underlying diseases
If you have an underlying condition that makes fatty liver disease more likely, such as diabetes or high blood pressure, keep these well-managed, with the help of your doctor. This can improve your fatty liver.
Losing weight
If you have fatty liver disease and are overweight, gradually losing weight should help your liver recover. Eating less and exercising more will help you lose weight. Aim to exercise moderately for at least 30 minutes, five days a week.
Medicines under investigation
There are many different medicines that are currently being researched for the treatment of fatty liver disease. However, these have yet to be shown to work. Some examples are listed below.
Vitamin E supplements. This may in specific populations, but more research is needed to prove if it is useful. Statins. These cholesterol-lowering medicines may help treat NASH. Metformin. This medicine is used to increase insulin sensitivity and may help in people with NASH. This class of drug has been linked with heart disease, so trials are looking at how safe it is. Ursodeoxycholic acid is a medicine used to reduce the production of bile acids. It is being tested for treating NASH. Omega-3 fatty acid supplements may reduce triglyceride levels. Surgery
Some research shows that surgery for weight loss may improve NASH.
Preventing alcoholic liver disease
The best way to avoid getting ALD is to avoid drinking .
However if you have been diagnosed with fatty liver or ALD, you should stop drinking completely.
Preventing non-alcoholic fatty liver disease
Although you cannot always stop NAFLD developing, the best way to reduce your risk is to maintain an active lifestyle and a balanced and varied diet to prevent you from becoming overweight.
 Parsi Teb Physical and Mental Health Journal
Parsi Teb Physical and Mental Health Journal